On March 10 McGill University hosted the final event of Concordia University’s Community Lecture Series, “Ending HIV/AIDS.” The main speaker was M-J Milloy, an infectious disease epidemiologist and assistant professor at the University of British Columbia and Principal Investigator of the AIDS Care Cohort to Evaluate Access to Survival Services (ACCESS). Although the talk was called “Ending HIV/AIDS” Milloy focused largely on HIV, speaking about the rise and decline of its prevalence in Vancouver’s Downtown Eastside.
Milloy said in his talk that in the mid-1990s, Vancouver saw the worst HIV outbreak ever observed in the Western world: within 12 months, the level of HIV infection in Vancouver’s Eastside went from 1 in 100 individuals to 1 in 4. Milloy said that this rise stemmed primarily from a shift from heroin, which is often injected up to five times a day, to cocaine, which can be injected up to 50 times a day. A rise in the demand of needles led to a decrease in supply, encouraging needle sharing.
Those hit hardest by the crisis were men who had sex with men (MSM), Indigenous peoples, people who were incarcerated, and other disadvantaged groups, a trend that has persisted to this day, noted Milloy.
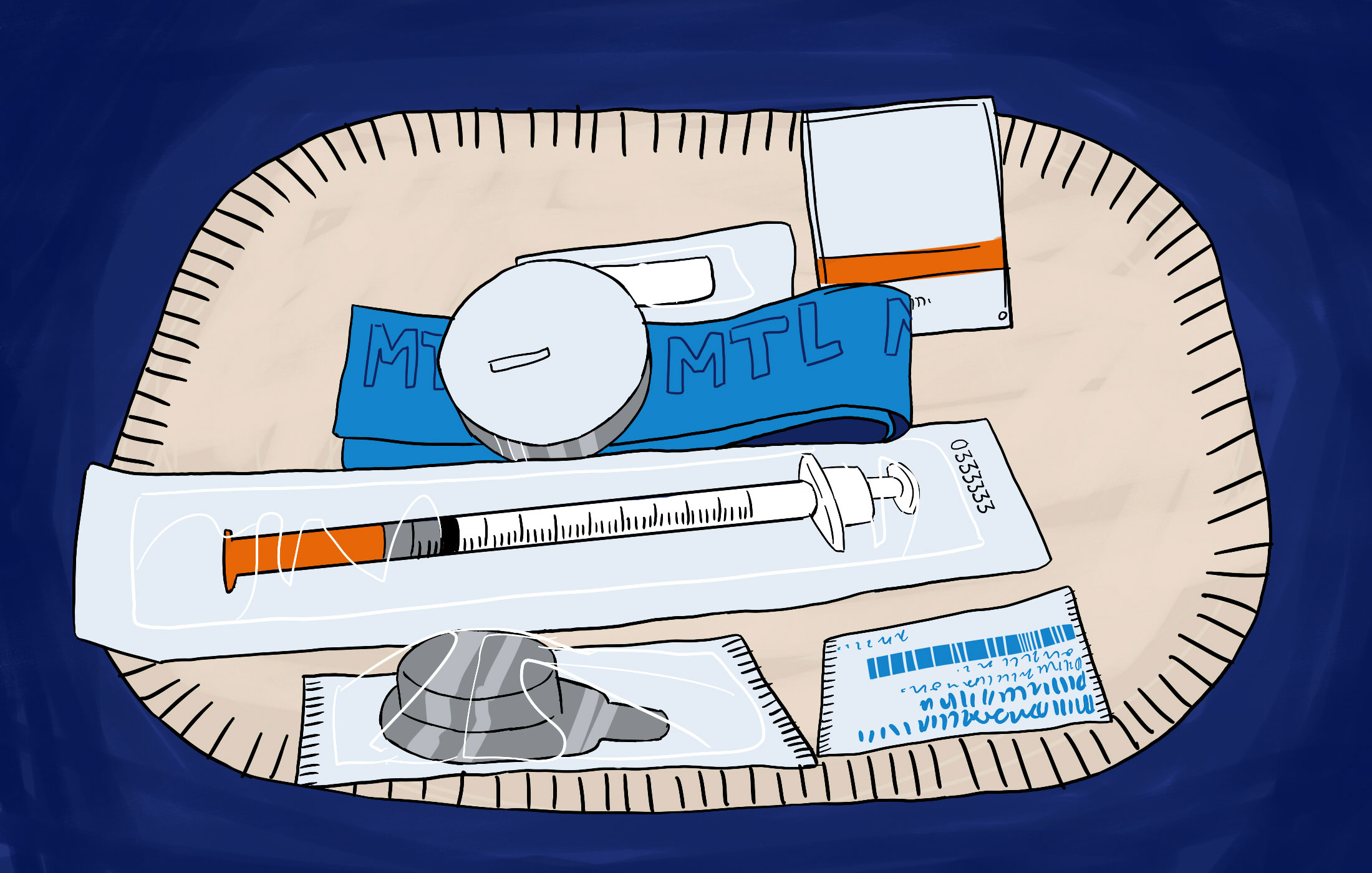
“The vast majority of people we work with are marginalized and there exist many barriers in their accessing social services,” said Geneviève Fortin, a representative from CACTUS Montréal, a Montreal community organization with needle exchange and collection services. “Many suffer from homelessness, mental health issues, and live in extremely precarious situations,” Fortin continued.
“What our scientists and I have concluded is that what really happened in Vancouver was not as much a story of drug use as much as it was a story about deadly public policy,” said Milloy.
He elaborated that the HIV crisis in Vancouver was exacerbated by the effects of a “public order-based” response to drugs: the fear of arrest and heightened stigma surrounding drug use pushed drug users away from healthcare facilities, resulting in less medical help for drug users. Correctional facilities lacked harm reduction initiatives and effective HIV/AIDS treatment.
Regarding the low rate of HIV infection in Vancouver today, Milloy said, “This was not a quirk of nature, but rather very specific actions [that] were taken during the outbreak which led us to the point where we could actually believe we could end the disease.”
These actions included a reorientation of Vancouver’s public safety agenda, with the city’s Health Board declaring a state of public health emergency, and adopting harm reduction initiatives to curb future drug use. Harm reduction can be defined as a policy that does not prohibit or eradicate a harmful act itself, such as drug use, but works to reduces the harmful effects of it.
Insite, the first legal supervised drug injection site in North America, opened in 2003 in Vancouver’s Downtown Eastside. Unlike a hospital or free clinic, Insite presented itself as “low-barrier,” allowing for a judgement-free zone where drug users were not afraid to seek out treatment. Over the next decade, some studies showed a 35 per cent decrease in the rate of fatal overdoses in the neighborhood.
Clinics like Insite saw opposition from both provincial and federal Conservative governments, who believed that harm reduction techniques were encouraging drug use in urban areas.
Even today, cities like Montreal grapple with the political challenges of setting up safe injection sites.
“The Harper government lost their attempt to close Insite in 2011,” said Milloy. “In response, what they did was pass Bill C-2, a federal law governing the opening of new facilities. [The bill] made it very difficult to [open new facilities], putting in a lot of unjustified conditions in front of organizations who wanted to open.” For example, letters from chiefs of police were required, but law enforcement agencies are traditionally against harm reduction methods.
Milloy concluded by saying that little additional research was needed to eradicate HIV in Canada.
“If I leave you with one idea from this talk, it’s that eradicating HIV among drug users is no longer a medical concern,” said Milloy. “We no longer need to figure out the medical tools to end this pandemic.”
He continued, “What Vancouver shows is that we need the political will to do something. We need politicians with the political will, who will not only devote the resources required, but who will also dismantle the structures of stigma, discrimination, criminalization and impoverishment which lead to HIV in these communities.”